What Is Gynecomastia?
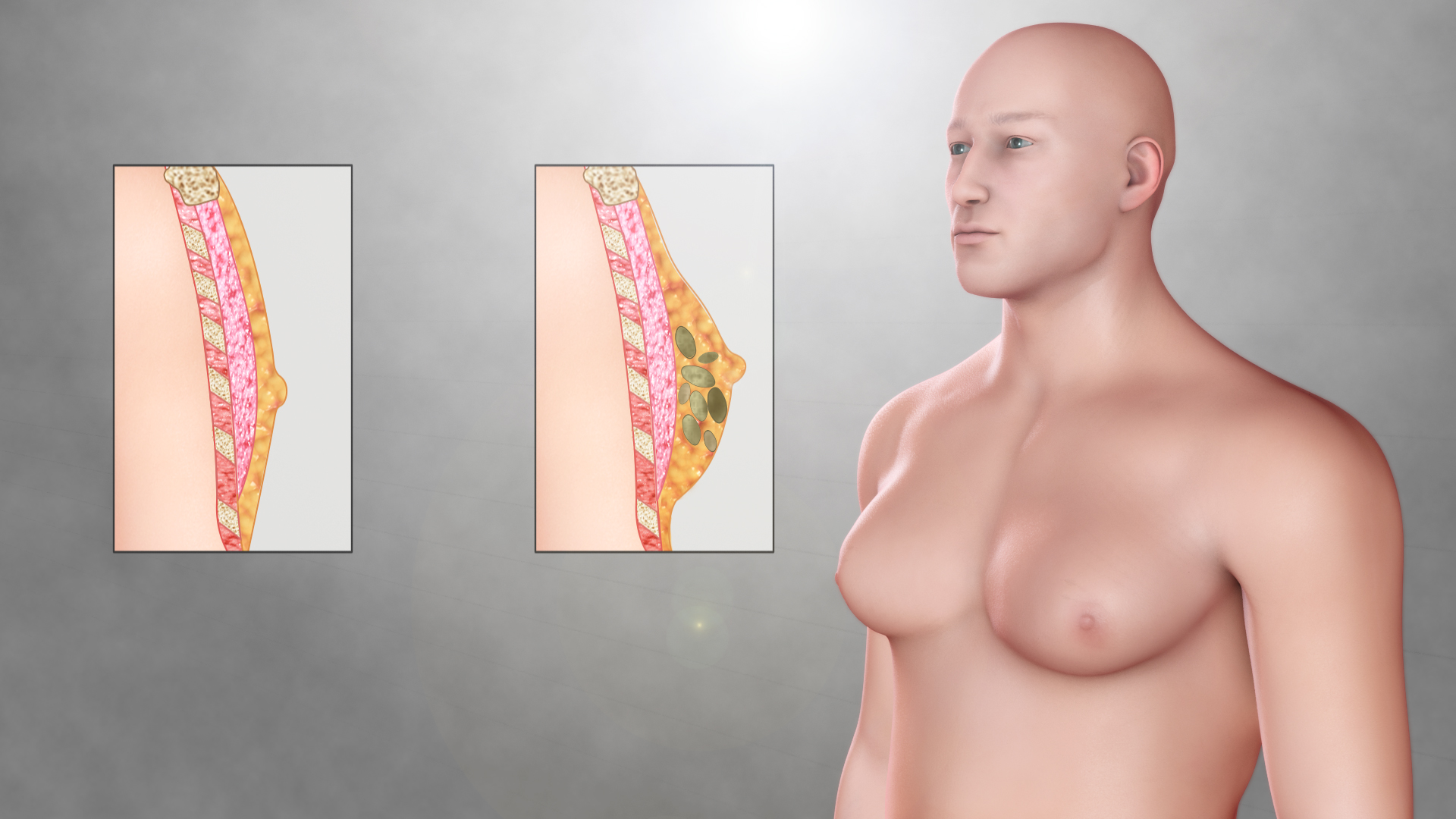
Gynecomastia is a benign enlargement of the male breast tissue caused by an imbalance between the hormones estrogen and testosterone. While both hormones are present in all sexes, testosterone typically predominates in males. However, when this hormonal balance is disrupted, estrogen can exert more influence, leading to the development of excess breast tissue in males.
Gynecomastia may affect one or both breasts and can occur at various life stages—during infancy, adolescence, or older adulthood. While not usually a serious medical condition, it can cause emotional distress and affect self-esteem.
Types of Gynecomastia
There are three distinct types of gynecomastia, typically categorized by the duration and tissue changes:
-
Florid gynecomastia: This early-stage condition (less than four months) is characterized by increased ductal tissue and vascularity. It’s the most treatable phase.
-
Intermediate gynecomastia: Considered a transition phase, this type lies between florid and fibrous stages.
-
Fibrous gynecomastia: Occurring after a year or more, this phase presents with dense, fibrotic tissue and is less likely to resolve without intervention.
Common Symptoms
The hallmark symptom of gynecomastia is the swelling of breast tissue in one or both breasts. Additional symptoms include:
-
Breast tenderness or pain
-
Sensitivity in the nipple area
-
Firmness under the nipple
-
Asymmetrical swelling (one breast larger than the other)
While most cases are not painful, some individuals may experience irritation or discomfort due to clothing friction. Any unusual signs like rapid swelling, nipple discharge, or bleeding should prompt immediate medical evaluation.
What Causes Gynecomastia?
Gynecomastia may arise from various causes, often related to hormonal changes. These include:
-
Infancy: Transient gynecomastia in newborns due to maternal estrogen.
-
Puberty: Hormonal fluctuations during puberty may trigger temporary breast growth.
-
Aging: Declining testosterone levels in older men can shift hormonal balance in favor of estrogen.
-
Medications: Certain drugs—such as anti-androgens, anabolic steroids, antibiotics, anti-ulcer agents, and some psychiatric drugs—can cause hormone imbalances.
-
Substance use: Alcohol, marijuana, amphetamines, heroin, and anabolic steroids are known contributors.
-
Health conditions: Disorders that affect hormones, such as hyperthyroidism, hypogonadism, tumors, kidney failure, and liver cirrhosis, can also lead to gynecomastia.
In some cases, the condition is idiopathic, meaning no specific cause is identified.
Risk Factors
Several factors may increase the likelihood of developing gynecomastia:
-
Age (especially during puberty and after age 50)
-
Use of certain prescription or recreational drugs
-
Chronic diseases affecting hormonal balance
-
Obesity (which increases estrogen production)
-
Family history of hormone-related disorders
Diagnosing Gynecomastia
To determine if someone has gynecomastia, a healthcare provider will typically begin with a thorough medical history and physical exam. Key steps in diagnosis include:
-
Medical history review: Inquiries into medications, drug use, onset of symptoms, and presence of pain or discharge.
-
Physical exam: A hands-on examination to distinguish true glandular enlargement from fat accumulation (pseudo-gynecomastia).
-
Blood tests: These check hormone levels, liver and kidney function, and thyroid status.
-
Mammogram or ultrasound: Imaging is used if a lump is detected to rule out breast cancer.
-
Testicular ultrasound: May be conducted to detect underlying testicular tumors or abnormalities.
Treatment Options
Treatment for gynecomastia depends on the underlying cause and duration of the condition:
-
Watchful waiting: In adolescents, the condition often resolves spontaneously within six months to two years.
-
Medication adjustments: If gynecomastia is drug-induced, switching or stopping the causative medication may help.
-
Hormonal therapy: Medications such as tamoxifen or raloxifene, though not FDA-approved for this use, can help reduce breast size.
-
Surgery: In cases of persistent or severe gynecomastia, surgical removal via liposuction or mastectomy may be recommended.
-
Compression garments: These can help reduce the appearance of breast tissue and improve confidence.
Preventing Gynecomastia
While not all forms of gynecomastia are preventable, there are steps individuals can take to lower their risk:
-
Avoid anabolic steroids and illicit drugs.
-
Limit alcohol intake.
-
Use medications responsibly and consult a doctor if breast changes occur.
-
Manage weight and maintain overall hormonal health.
-
Address any underlying conditions that may disrupt hormone balance.
Related Conditions
Gynecomastia may be associated with or resemble other conditions, such as:
-
Pseudogynecomastia: Fat accumulation without glandular growth, common in overweight individuals.
-
Breast cancer: Rare in males but possible; any hard, fixed, or rapidly growing mass should be evaluated.
-
Hyperthyroidism
-
Testicular or adrenal tumors
-
Klinefelter syndrome: A genetic condition affecting male hormone levels
Living With Gynecomastia
The emotional and psychological impact of gynecomastia can be significant. Many men feel embarrassed or anxious, which may lead to social withdrawal and reduced self-confidence. Strategies for coping include:
-
Open discussion with healthcare providers for treatment options
-
Support from friends, family, or peer groups
-
Online communities, such as Gynecomastia.org, for shared experiences
-
Consultation with a mental health professional for emotional support
When To See a Doctor
See a healthcare provider if:
-
Swelling persists or worsens
-
There is pain, discharge, or bleeding
-
You notice a firm or immobile lump
-
Breast changes are accompanied by other health symptoms
Early evaluation can rule out serious causes and help guide treatment.